This is featured post 1 title
Replace these every slider sentences with your featured post descriptions.Go to Blogger edit html and find these sentences.Now replace these with your own descriptions.

This is featured post 2 title
Replace these every slider sentences with your featured post descriptions.Go to Blogger edit html and find these sentences.Now replace these with your own descriptions.

This is featured post 3 title
Replace these every slider sentences with your featured post descriptions.Go to Blogger edit html and find these sentences.Now replace these with your own descriptions.

Monday, November 26, 2012
Hallux varus
o Congenital
o Trauma
o Sometime Bunion surgery (swelling of joint between great toe and 1st metatarso - pharyngeal joint)
o Deformity
o Pain
o Decrease ROM
o Problems with shoe wear
o Clawing of great toe
Depends on severity, if deformity is mild and the toe remain flexible, no treatment is required.
Genu Valgum
It
is also called knock knees. It is a condition in which the knee angle
is in and they touch each other when the legs are straightened. Females
have a wider pelvis than males and relatively shorter length of thigh
bone and as a result have a greater static genu valgum than men.
Individuals with severe Valgus deformity are typically unable to touch
their feet together while simultaneously straightening the legs. Valgus
actually mean bent outwards. But here the distal portion bends outwards and the proximal portion seems bend inwards.
Causes:
i. Idiopathic
ii. Congenital
iii. Osteogenesis imperfecta
iv. Rickets
Diagnosis:
· X – rays
Management:
Medical treatment for Rickets is optimum vitamin D, for Osteogenesis imperfecta is Bisphosphonates.
Surgical options:
Osteotomy using extaperiosteal two holes plate for 12 month, sometimes repeated osteotomies might be required.
Genu vara
It
is also called bow legs. There is a medical angulation of leg in
relation to thigh. There is outward curvature of femur and up to the age
of 3 – 4 years children have a degree of varus normally.
Causes:
1. Rickets
2. Infections
3. Tumor
Management:
· One should always identify the cause and if possible should be treated.
· Surgical osteotomy (Multi – disciplinary team)
Proximal Femoral deficiency
Basically there is proximal femoral deficiency, the proximal femur is partially absent and the entire limb is shortened.
Frequency:
Etiology:
· No exact known cause
· Injury to neural crest cells (embryonic cells of spinal cord and brain)
· Defect
in proliferation and maturation of chondrocytes in proximal growth
plate due to anorexia, ischemia, irradiation, bacterial, viral
infection, toxins, hormones, mechanical injury, thermal injury,
thalidomide (anticancer drugs). No genetic etiology. There is associated
high incidence of other anomalies like fibula deficiency, Valgus feet,
cleft palate, and club foot.
AITKEN classification of proximal femoral deficiency:
AITKEN divided it into the following four categories.
Class A:
Femoral head is often absent
Class B:
Femoral head is absent + proximal femur
Class C:
Absent femoral head dysplastic acetabulum, tronchanter doesn’t develop.
Class D:
Remember in the 1st two categories ossification may occur
Diagnosis:
Radiographic studies
Management:
· Prosthesis (head of femur)
- Treatment is delayed in child after 3 years.
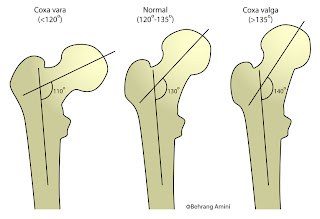
Coxa valga
Normally the angle between the head of femur and shaft is 120° - 135°. An angle above 135° is coxa valga.
Causes:
1) Skeletal disease (Osteomyelitis, Paget’s disease, Osteogenesis Imperfecta)
2) Spasticity of adductor muscles of hip
3) Cerebral palsy (a
disorder of movement and or posture as a result of permanent damage to
the developing brain. This damage may occur before, during, or
immediately after the delivery and has many causes)
4) Spinal dystrophism (Spina bifida)
5) Poliomyelitis
(an infectious virus disease affecting the CNS. The virus responsible
is RNA, transmission through orofaecal, and 90 – 95% polio affected
people will not develop polio disease)
Management:
Non surgical:
a. Physiotherapy:
Aim is stretching the spastic agonist muscles.
b. Orthotic devices:
These help in maintaining adequate positioning
Surgical:
Valgus osteotomyCoxa vara
Normally the angle between the head of femur and shaft is 120° - 135°. An angle below 120° is coxa vara.
Causes:
1) Trauma
2) Congenital
3) Paget’s disease (also
known as osteitis deformans ,a chronic disease of bones, occurring in
the elderly and most frequently affecting the skull, backbone, pelvis,
and long bones. There is 1% risk to develop osteosarcoma. Treatment is
with bisphosphonates or calcitonin)
4) Perthes disease (avascular
necrosis, decrease supply to the epiphyseal plate of femur or necrosis
of head of femur due to interruption of its blood supply)
5) Osteomyelitis (inflammation of bone due to infection)
6) Osteogenesis imperfecta (fragilitas
ossium is a congenital disorder in which the bones are usually brittle
and fragile. No treatment, there is abnormal; collagen type I, type II,
type III, and type IV. Patient involving type I, IV live normal, with
type II die early and with type III has severe disease.)
Symptoms:
In unilateral condition the limb may be small. There will be gait problem.
Diagnosis:
Radiological:
o X – rays
o MRI/CT scan
Treatment:
· Varus Osteotomy
· Hip dynamic screws
· One should identify causes and if possible should be treated
· Physiotherapy
Intoeing
In
this condition the front half of the foot is deviated inwards contrary
to Talipes Equinovarus which is deviation at the ankle. In this
condition the ankle is spared.
Intoeing
between the ages of one and two ears is usually a result of an abnormal
in alignment of upper (thigh) and lower leg. While Intoeing developing
around 18 months may be the result of abnormality in pelvis and hip.
 |
| Intoeing |
Causes of intoeing:
1) Neurological abnormality (Cerebral Palsy, Multiple Sclerosis, Polio etc)
2) Metatarsus adductus (A foot deformity in which the bones in the front half of the foot bend or turn in toward the body)
3) Hallux Varus (medial deviation of the great toe)
4) Club foot
5) Pes cavis (high instep arch)
All of these exhibit intoeing between the ages of 1 to 2 years. The abnormality is in alignment of upper and lower leg.
Management:
Casting:
· Applied at 6 months beneficial up to 2 years
· Success rate drops dramatically after age of two years
Surgery:
· Ligaments released
· Metatarsal Osteotomy
Physiotherapy
Talipes Equinovarus (Clubbed foot)
It
is a congenital deformity involving one or both feet. The affected foot
appears rotated internally at ankle. The person appears to walk on
their ankles. Approximately 50% are bilateral. It occurs commonly in
female i.e. 2:1
Causes:
· Edward syndrome (extra chromosome on 13 number)
Management:
a. Tenotomy:
Need in 80% cases
b. Anterior tibial tendon transfer:
The tendon is moved from first toe to 3rd in order to release inward traction on foot.
c. Ponsiti method:
It is a conservative approach in which serial cast applied over 4 weeks then Mini incision in Achilles tendon.
PhysiotherapyNeural tube defects
It
is an embryonic tissue which covers the brain and spinal cord. The
defect in neural tube can involve the cranial (cephalic) or the caudal
end. It can be mild, moderate or severe.
Anencephaly:
When
the head (cephalic) end fails to close resulting in absence of major
portion of brain and skull is called anencephaly. Infants born with this
condition are usually blind, deaf and unconscious. They die within few
hours and days after birth.
Encephalocele:
Sac like protrusion of brain through opening in skull is called encephalocele.
 |
| Encephalocele |
Spina bifida:
A
condition which involves the caudal end of neural tube is called spina
bifida. There is incomplete development of spinal arch. It can be
divided into the following types.
Spina bifida occulta:
It
is the mildest form (hidden spine deformity). Most patients have never
any health problem. Rarely the skin has moles, hair tufts. Sometimes the
spinal cord or nerves are tethered to the spine. The abnormality may
involve single or multiple vertebrae which may need surgery.
 |
| Types of Spina Bifida |
Spina Bifida Cystica:
Meningocele: The meninges (sac) protrude through opening.
Meningomyelocele: Both meninges and spinal cord protrude.
Causes:
a. Genetic factors
b. Folic acid deficiency
c. Drugs (Valporate, Methotrexate)
d. Smoking
Management:
· Physiotherapy
· Neurosurgery (definitive)
Sprengel's deformity
A
developmental abnormality in which the scapula doesn’t descend to its
proper position or a high lying shoulder blade is called sprengel's
deformity. In the intrauterine life it is lying in the cervical region
then it descends. The associated muscles may be weak (trapezius,
rhomboid muscles etc).
 |
| Sprengel's deformity |
Presentation:
· Shoulder asymmetry
· Restricted shoulder abduction
· Scapula is adducted and 2 – 10 cm elevated.
· Inferior pole is deviated medially, the glenoid faces inferiorly, and the length of vertebral border is decreased.
Associated problems:
· Poland syndrome
· Klippel-Feil syndrome (short, webbed neck; decreased range of motion (ROM) in the cervical spine)
· Scoliosis
Cavendish classification:
Based on the severity of the condition, a Sprengel deformity can be classified as follows (Cavendish grades).
Grade 1:
The deformity is very mild with clothes it cannot be seen. The shoulders are almost at level.
Grade 2:
This is mild deformity but the superomedial portion of the high scapula is visible as a lump.
Grade 3:
It is a moderate deformity. The affected shoulder is 2 – 5 cm higher than the opposite shoulder. It is visible.
Grade 4:
It is severe deformity. The scapula is very high with neck webbing and brevicollis.
Diagnosis:
Imaging Chest X – ray:
To confirm the diagnosis and to look for associated anomalies.
CT – Scan (thorax):
Omovertebral body can be seen, which is a bony bar that attaches the scapula to spine (cervical).
Management:
· Physiotherapy to gain mobility
· Definitive treatment is surgery
· Repositioning of the scapula is done (modified green scapuloplasty and wood ward procedure)
Scoliosis
In this condition the spinal cord look C – shape.
Causes:
1. Idiopathic
2. Genetic factor play important role
Clinical features:
· Uneven musculature on affected side
· Prominent shoulder blade
· Uneven hips, leg length, lung and heart can be affected
Associated conditions:
i. Charcot Marie tooth disease
ii. Prader – willi syndrome
iii. Ehleros danols syndrome
iv. Marfan syndrome
v. Arnold chiari malformation
vi. Kyphosis
 |
| Scoliosis |
Diagnosis:
History, examination, X – ray, MRI and look for associated conditions
Management:
· Surgery
· Physiotherapy
· Occupational therapy
Flat feet (Pes Planus)(Fallen Arch):
The
arch of the foot collapses, the entire sole coming into complete or
near complete contact with ground. In 20 – 30 % of the population, the
arch never develops unilaterally or bilaterally. Children usually have
flat feet but as they grow it will correct by itself.
Management:
· Most of the cases don’t require treatment
· Arch support (orthotic)
· Surgery: It is the last resort. It is also costly and time consuming.
Torticollis
Involuntary
contraction of neck leading to abnormal posture and movement of head is
called Torticollis. It is not a diagnosis but a sign of underlying
disorder.
Causes:
1. Congenital
2. Acquired
1. Congenital:
· Trauma (by birth) to sternocleiodomastoid
· Spina bifida
· Vertebral anomalies
· Clavicle fracture
· Arnold
– chiari malformation (protrusion of lower brain stem and cerebellum
through the opening for spinal cord at the base of the skull)
2. Acquired:
o Spasm of cervical muscles due to injury to muscles or nerves
o Awkward position during sleep
o Cervical spine trauma
o Retropharyngeal abscess
o Any infection involving surrounding tissue of neck
o Drugs: Phenothiazines (piprazine), Metachlopromide
Diagnosis:
§ X – ray of neck
§ MRI/CT of spine
Management:
General:
· Check airway
· Patient with trauma stabilize neck
Remember: Cause identification is primary aim and then treatment accordingly.
Specific:
· Benztropine
· Benzodiazepine
· Analgesics
· Physiotherapy


 8:22 AM
8:22 AM
 Aftab Ahmad Khan Yousafzai
Aftab Ahmad Khan Yousafzai